Black mothers in the UK are five times more likely to die from direct and indirect complications during childbirth than their white counterparts.
MBRRACE‐UK released its annual report in November 2018 on the UK and Ireland Confidential Enquiries into Maternal Death and Morbidity. The report looks into the leading causes of maternal mortality rates in the UK and Ireland.
In its findings, MBRRACE-UK states the leading direct and indirect causes for maternal deaths such as haemorrhage, cardiac arrest, suicide, and even includes homicide. Solutions offered in the report include beginning treatment early on in pregnancy and continuing through the first 12 weeks postpartum. Other solutions include better training and intake practices by medical staff.
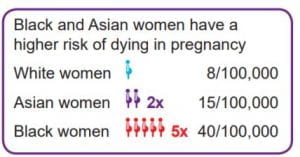
MBBRACE-UK report findings show disparities among Asian and Black women dying from complications of pregnancy at higher rates than their White counterparts. Source: MBBRACE- UK 2018 Confidential Enquiry into Maternal Death report
Glossed over are the racial disparities found between mortality rates for women of colour and their white counterparts. The report found that Asian women are two times more likely to die from pregnancy complications, and the statistics for Black women fare out worse.
The report found that Asian women are two times more likely to die from pregnancy complications, and the statistics for Black women fare out worse.
However, there is no further research or solutions offered for these statistics and the report moves on to risk factors that affect older pregnant women.
While the report published states the tangible medical reasons why women are dying, it fails to mention racial biases that contribute to those deaths.

Professor Marian Knight, Professor of Maternal and Child Population Health at the National Perinatal Epidemiology Unit, Nuffield Department of Population Health Photo courtesy of British Maternal and Fetal Medicine Society.
Professor Marian Knight, Professor of Maternal and Child Population Health at the National Perinatal Epidemiology Unit, Nuffield Department of Population Health, who led the study for MBBRACE-UK, supports the claims that actions need to be taken to prevent maternal deaths. This includes having better-trained doctors and emergency plans, both claims that were included in the MBBRACE-UK study.
Knight also believes that there needs to be better connections between patients, doctors, and specialists; something that is lacking as of now.
One of the reasons Knight believes that racial bias is prevalent in the medical field is the lack of communication and compassion. She notes that a language barrier and lack of access to medical care can cause unnecessary risk to expecting mothers. When a language barrier exists or access to medical care is difficult small problems may go unnoticed until too late, putting both mother and child at risk.
Another factor at play against being black mothers is not being listened to or being taken seriously by medical staff when expressing concern about their health. This takes a toll on mothers who have expressed anxiety over potential racial bias in the health system and choose not to bring up their concerns.
But even when a black woman expresses her concern she may be ignored or told she is worrying ‘too much.’ Dr Ria Clarke, who is training to be a consultant in Obstetrics and Gynaecology, states that the best way to figure out the reasons that black mothers are dying at higher rates is to talk to mothers about the treatment they are receiving, then taking the findings from those testimonials and improve treatment to fit the conversation.