A recent seminar for Forth Valley, the catchment area that includes Stirling, Clackmannanshire, and Falkirk, showed that drug deaths were at an all time high, sitting at a total of 69 deaths for this area alone.
Following the July publication of the National Records of Scotland’s ‘Drug-Related Deaths in Scotland in 2018’, which showed yet another catastrophic rise in drug deaths across the country, the Alcohol and Drug Partnership, ADP, has began hosting local seminars targeting problems that face particular areas and constituencies.
This increase in deaths placed Forth Valley above the national average of 0.219 deaths per 1000 of population, with 0.225 deaths per 1000 of local population.
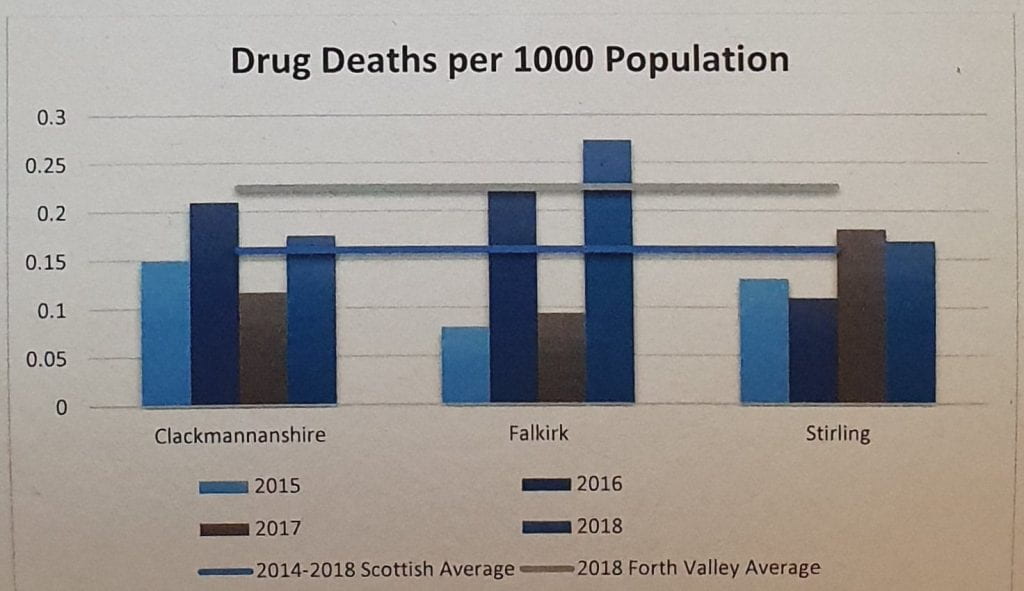
Variations from the national average also appeared in terms of the victim’s age. The mean age of Forth Valley victims was 39.4 years, falling a couple of years below the national average of 42. This is partly due to the victims being aged between the ages of 25 and 34, which was much younger than the national aging cohort average of 35 to 54.
Also growing in line with national averages was the cause of death being linked to polydrug abuse, meaning that the drug deaths were linked to multiple types of drugs being in the victim’s system.
In all Forth Valley cases polydrug use was discovered in the user’s systems, with the average number of substances found sitting at around 4.75. The most popular of these drugs included benzodiazepines, appearing in 83% of the deaths; opioid substitutes at 62%; and heroin or morphine appearing at 61%.
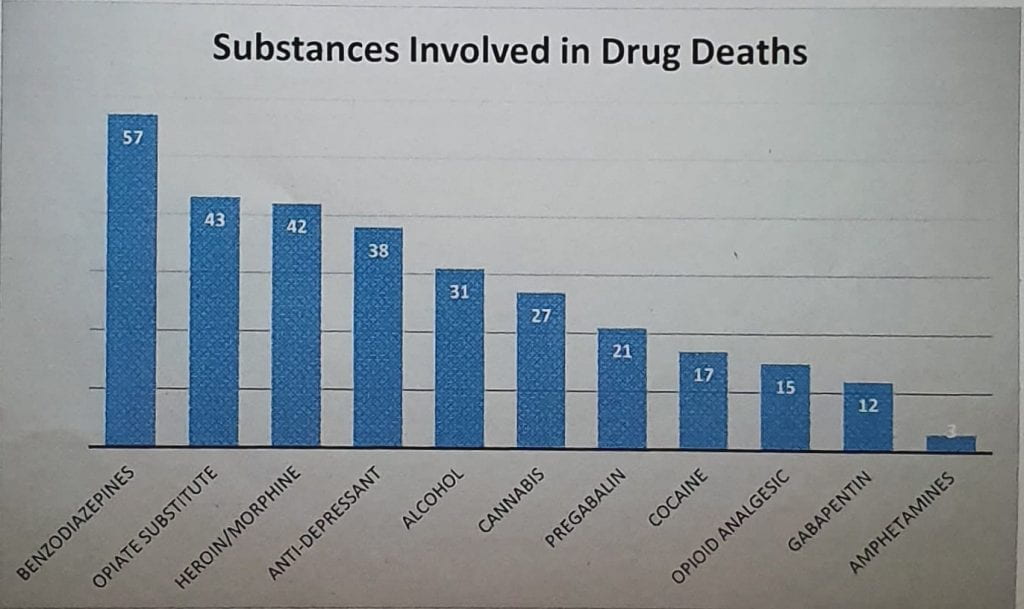 All three of these drugs classes can be prescribed by GPs, but in all cases either a quarter or more of the victims had illicitly procured them. This is particularly evident in Falkirk where 34 of the 44 deaths were found to have benzodiazepines in their system.
All three of these drugs classes can be prescribed by GPs, but in all cases either a quarter or more of the victims had illicitly procured them. This is particularly evident in Falkirk where 34 of the 44 deaths were found to have benzodiazepines in their system.
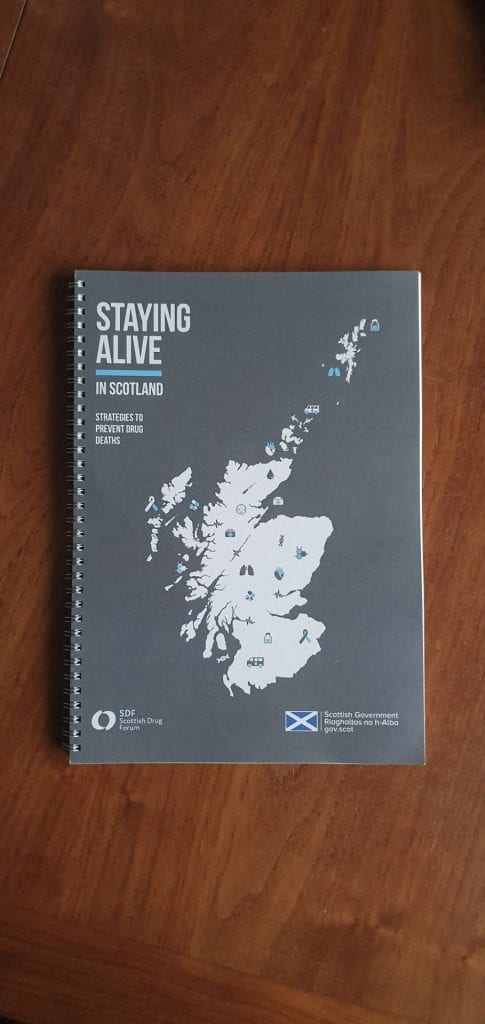
As a response to the increase of drug deaths nationally, The Scottish Drugs Forum have created a new toolkit which aims to prevent drug-related deaths.
The 2019 edition of ‘Staying Alive in Scotland; Strategies to Prevent Drug Deaths’ is an update to the SDF’s 2016 toolkit of the same name. Published in conjunction with the Scottish Government the toolkit outlines ways in which doctors and healthcare specialists can reduce drug-harm, and work with existing avenues of recovery to develop the physical and mental resilience of those in pre-existing programmes.
Spanning over 14 chapters, the toolkit offers information, work-sheets, and guidance to professionals on how to improve the effectiveness of their practice and improve their care.
“Staying Alive is focused on immediate changes that the health service can make, most of them not too expensive, in order to make the health service more accessible across the board, even to those who usually find it difficult to access those services.” Mariebeth Kilbride, Senior Office for Drug Prevention with the SDF explains.
This idea of accessibility to health services is the central message of the toolkit, with a lot of focus on how mental health treatment, particularly, should be encouraged as part of a well rounded treatment plan, but there is still ways to go.
“Mental health services and drug treatment services have never been fully integrated in Scotland, some areas such as Forth Valley have done better than others, but it has been traditionally really difficult to get people that use drugs into mental health treatment.”
This is partly due to mental health services wanting to treat patients who are as stable as possible, but as Kilbride points out “because of the trauma involved in most people who take drugs it is very difficult to achieve that level of stability without mental health support, it becomes a sort of chicken and egg situation.”
The SDF is also campaigning for intramuscular drug Naloxone, a drug that can be used to prevent opioid overdoses, being more widely accepted across Scotland as a whole. Also found as an intranasal drug ‘Nixoid’, which was only recently introduced to Scotland in February, both drugs could help with harm reduction.
“There is a lot of myths and stigma around Naloxone, but since 2015 anyone in Scotland is allowed to carry a naloxone kit if they are likely to witness an overdose… Across Europe for every fatal overdose there is 25 prevented ones, when extrapolated to Scotland even if that number is not the exact same, it gives perspective of how likely Naloxone is to save lives.”
“What I would like to see us get to is the stage that they have in places like Canada where it has almost became a social responsibility to carry Naloxone… It is very much an effort based in protecting the community, that would be the ideal situation, to have kits placed all around, possibly even going as far as having a kit kept wherever there is a defibrillator to be found.”